|
Eligibility phone or video call
If you agree to be contacted about the study, you will receive a telephone, or video call, from the research team at your local hospital. The researcher will ask if you would like to take part in the study, answer any questions and confirm that you are eligible to participate.
Consent
If you decide to take part, you will be given a personal link to complete an online consent form.
The researcher will arrange an appointment to attend the rheumatology research clinic at your local hospital. This details of this visit are described below (visit one).
Completing a research questionnaire
We will ask you to complete a questionnaire online at the beginning of the study so we can see how your back pain is affecting you. This questionnaire might take around 25 minutes to complete.
Visit one
You will be sent details of your appointment once a date is confirmed. On the day of the appointment at your local hospital you will be met by a researcher who will guide you through all the assessments to be performed and confirm you are happy to continue with the study.
- The appointment will include a clinical assessment that will last around 30 minutes. The assessment will look for signs of arthritis, measure your mobility and ask about your personal and family history relevant to the condition.
- We will ask whether your pain eases after taking a non-steroidal anti-inflammatory medication (NSAID) such as ibuprofen for 7 days. If this is unclear, and it is safe for you to do so, the clinician will ask you to take a 7 day course of an NSAID medication. You will then be contacted at the end of the 7 days to ask whether the NSAID medication had any effect on your back pain.
- You will also provide a blood sample. The blood sample will be used to look for a genetic marker related to spine inflammation HLA-B27 (human leukocyte antigen B27) and CRP (c-reactive protein), high levels of which can show there is inflammation present in your body. The blood sample will be destroyed after analysis.
- You will also be asked if you would allow for samples of your blood to be stored for future research (this is optional and is part of a separate study).
- If you are aged 18 and over, an x-ray of your sacroiliac joints will be taken. These are the joints between your pelvis and lower spine.
- The researcher will arrange the second visit which will be for the MRI Scan.
Visit two
- You will attend the final visit at your local hospital for your MRI scan.
- It is important that you do not take any NSAID medication (eg ibuprofen, diclofenac, naproxen, meloxicam, etoricoxib, etodolac and nabumetone) for 7 days before your MRI as these can make the scans less clear. You can take other pain killers such as paracetamol if needed. The MRI should last around 30 minutes and will be of your sacroiliac joint and whole spine. You can restart your NSAID medication after the scan.
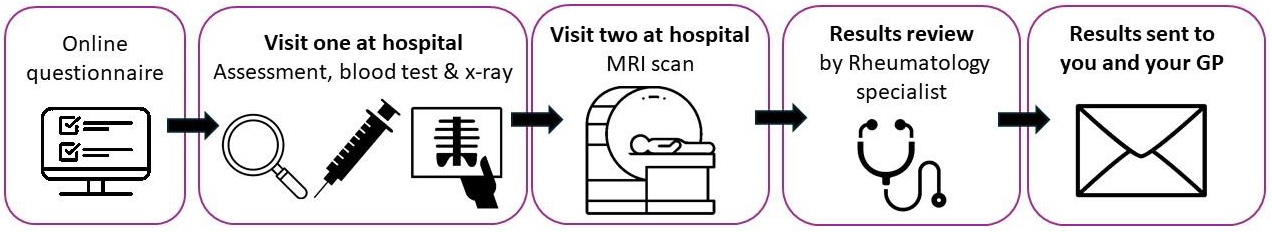
The results from your assessment, blood test, x-ray and MRI scan will be reviewed by a specialist who will make a decision whether your back pain is due to inflammation (i.e. you are highly likely to have axSpA) or not inflammatory (i.e. not due to axSpA). They will write to you and your GP and offer advice of the next steps for your treatment/care pathway.
We will inform your GP about your participation in this study.
Your name and telephone number will be shared with Esendex, our text messaging provider and their sub-processors, and will be used to send you text message reminders about the study and study questionnaires whilst you are participating in the study. Esendex will hold this information securely and delete it from their records at the end of the study.
We require contact to be maintained with you throughout the study, to arrange appointments and send you the results of the investigations at the end of the study. With your consent, we may send you further brief follow-up questionnaires (up to 3 years) [subject to additional funding – you will be informed if this will go ahead once funding has been confirmed.]. We will ask your permission to send you newsletters, final study results and information about future studies, this contact is optional.
As a thank you, if you attend the study visits, you will receive a £15 shopping voucher.
|